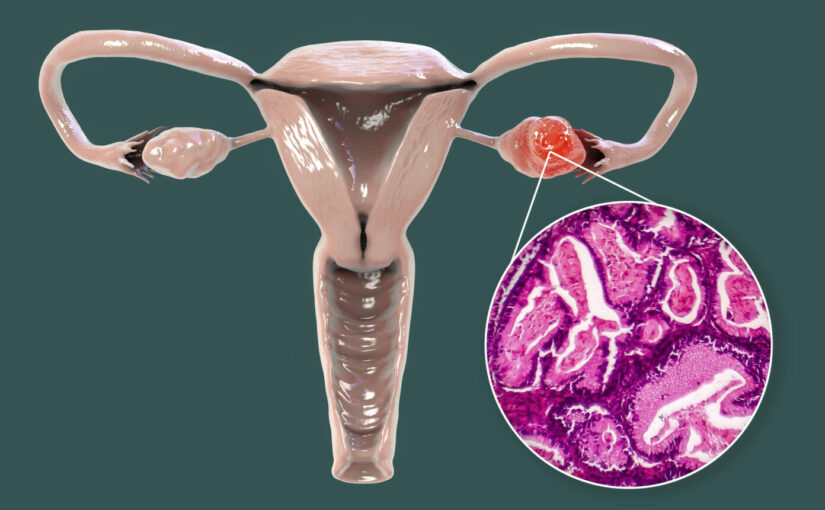
A new study describes a new diagnostic approach that could help identify the 15% of women with ovarian cancer whose tumors are intrinsically refractory to standard platinum-based therapies, the most common type of chemotherapy for the disease.
Most ovarian cancers are very sensitive to platinum therapy, at least initially. However, 15% of patients never respond and the field currently lacks any good screening tests for ovarian cancer—let alone for these patients. As a result, most tumors are detected in late stages of the disease and nearly all patients receive platinum-based chemotherapy.
“Unfortunately, by the time you see platinum therapies are not working, those patients are too sick to even be eligible to get them into a clinical trial,” explains Amanda Paulovich, of the Fred Hutchinson Cancer Center and co-senior author of the study published in Cell. “Their outcomes have not changed for decades.”
To predict those patients with refractory disease, the team performed a combined proteomic and genomic analysis on three different tumor cohorts: a discovery cohort, which included formalin-fixed paraffin (FFP) tumors sourced from four different academic repositories, and two validation cohorts, one of which was FFP, and the other was frozen tumors. In total, the team evaluated 242 ovarian cancers collected from patients before beginning treatment.
“Despite more than 30 years of literature on platinum resistance, not a single biomarker has been clinically translated and we think that is because there have been more than 900 genes and proteins implicated that map to lots of different cell pathways,” Paulovich explains. So instead of doing a traditional biomarker tissue study using immunohistochemistry (IHC) which assessed one protein at a time, the team looked for protein pathways at a network level.
The researchers identified a 64-protein signature after applying a novel technological approach involving targeted mass spectrometry coupled with machine learning. Specifically, they performed multiple reaction monitoring (MRM) mass spectrometry which focuses on proteins of interest, ignoring everything else in the background.
This approach sidesteps the limitations of starting with a training model or feature selection of individual genes and proteins. “Instead we utilize the pathway as a tool to build our prediction model so we better capture a lot of the important protein/protein interactions within the pathways,” adds co-senior author Pei Wang, of the Icahn School of Medicine at Mount Sinai. “We believe that system-level activity is very important for us to really characterize key features in those complicated tumors.”
Their ensemble prediction model identified 35% to 40% of tumors with platinum-refractory disease, which says with virtual certainty that the tumor will not respond to platinum. “It’s not 100% but it’s a stepping stone trying to get there until we can work with bigger patient cohorts,” adds Paulovich.
Beyond the discovery of the 64-protein signature, the research team identified five subtypes of ovarian cancer based on protein pathway expression that they believe represent different mechanisms of platinum refractoriness. “These are not individual protein markers, but distinctive protein pathways,” Paulovich says. The molecular changes at play in these newly defined ovarian tumor subtypes may represent targets for future treatments.
With this information, the team suggests a possible two-step precision oncology approach when assessing ovarian cancer. One, is the tumor platinum refractory? Run an MRM panel on these 64 proteins or some subset thereof, to figure out the probability of a refractory tumor before treatment starts. Two, if the tumor is refractory, perform a second panel to see what subtype the tumor is. That puts a patient into a treatment category based on the vulnerability of her tumor.
The diagnostic approach is still in its early stages and needs to be tested in larger cohorts. However, Paulovich and colleagues already published research in Cell Reports Medicine in 2021 showing they could replicate those five ovarian cancer subtypes in mouse models. One subtype in particular exhibited very high expression of a fatty acid oxidation protein. When they treated the mice with inhibitors of fatty acid oxidation, they restored platinum sensitivity to the mice. “That was a good preclinical model demonstrating that this approach was worth pursuing further,” notes Paulovich.
The team foresees that a clinical assay endpoint would look much like a score that indicates the likelihood of a platinum-refractory tumor and secondarily what class the tumor falls into. According to Paulovich “That would at least enable patients to participate in clinical trials that they haven’t been able to for decades because we haven’t been able to recruit enough patients with primary refractory disease into trials.”
This article was published by: Inside Precision Medicine