OCRA Expands Educational Programming with New Offerings
Ovarian Cancer Research Alliance is offering new opportunities for patients and survivors to connect, learn, and stay informed.
OCRA Expands Educational Programming with New Offerings
Ovarian Cancer Research Alliance is offering new opportunities for patients and survivors to connect, learn, and stay informed.
Only OCRA combines a laser focus with a panoramic view.
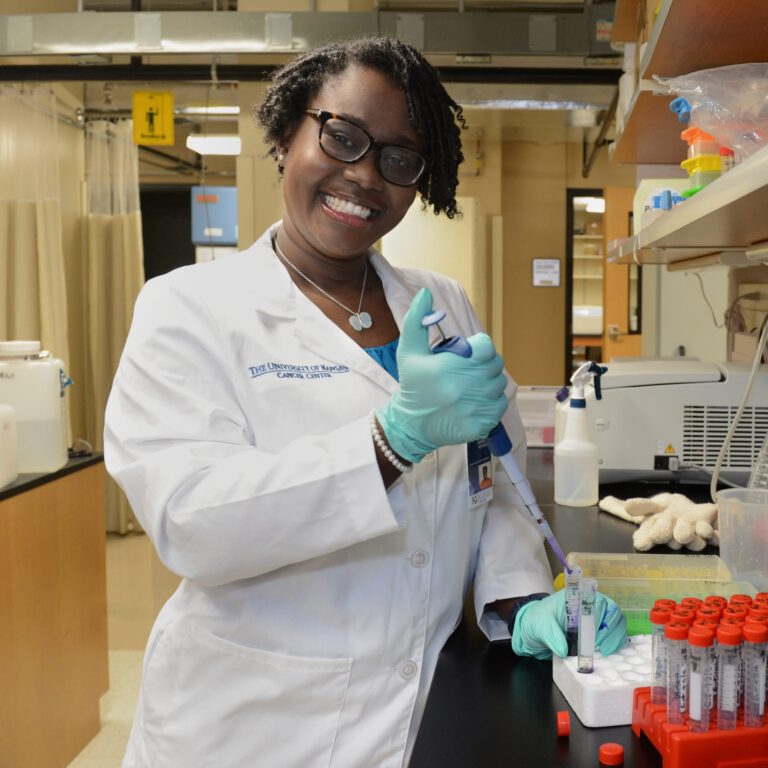
Funding Breakthrough Research
OCRA has invested $128 million toward finding a cure for ovarian and gynecologic cancers.
Discover our research
Supporting You Every Step of The Way
OCRA’s groundbreaking patient support programs help more than 95,000 people each year navigate an overwhelming diagnosis, aiding patients and families when they need it most.
Find support
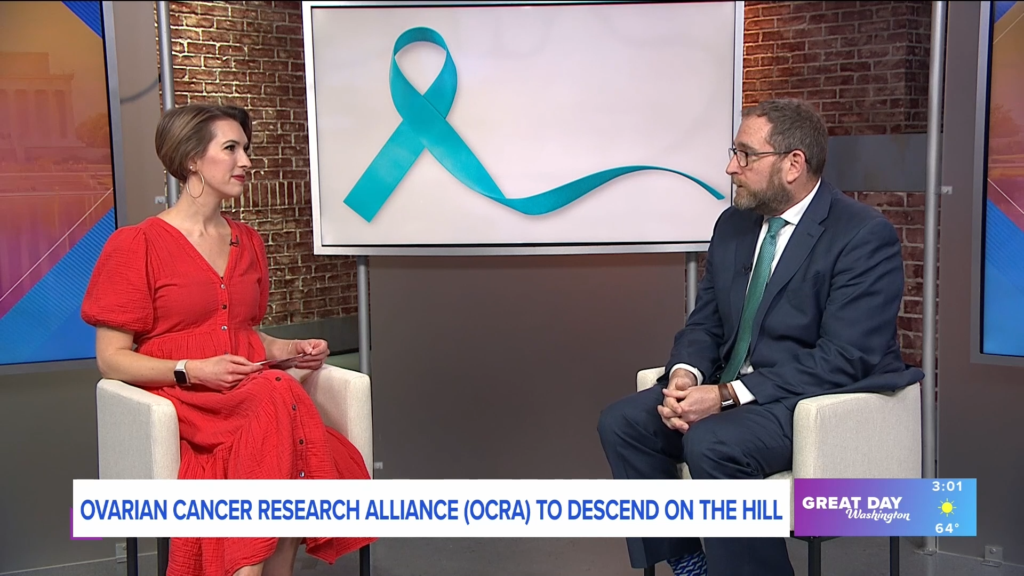
Advocacy is the Lifeblood of Change
OCRA advocates on Capitol Hill to improve research and education, drug and diagnostic safety, and access to quality care for all members of the ovarian and gynecologic cancer community. To date, OCRA has helped secure more than $3.8 billion in federal funding.
Take action now
Genetic testing can save your life.
Knowledge is power. Genetic testing can lower your risk of ovarian and gynecologic cancers.
The power of shared experiences
Join our Staying Connected Support Series, Woman to Woman Peer Mentor Program, or online community for knowledge, connection, support, and hope.