Medical science is more advanced than at any point in history. Yet the health care system — medical science applied to actual patients — still leaves many people without the best and latest treatments.
For example, new knowledge about health and disease accumulates in research labs at an accelerating rate. Genomics explores the effects of DNA variations. Proteomics examines the roles of proteins. The microbiome, the set of microscopic creatures living on and in us, is increasingly linked to well-being. And environmental influences affect all of these other factors, for good or ill.
But amid this torrent of discoveries, there’s a growing backlog in trying to put them into action. The innovations remain stuck in the laboratories or kept within elite medical institutions, left untranslated into medications, equipment and other therapies that would help doctors, health insurers and the public.
Fixing the bottleneck has become its own branch of medical science. The young but exploding field is known by various names that emphasize various nuances — translational medicine, personalized medicine, individualized medicine and precision medicine.
These terms point toward the same goals: Making medicine more effective by creating smoother and quicker paths for commercializing lab discoveries, plus tailoring those new products and technologies to the many different types of patients.
“In its simplest terms, it’s the right drug for the right patient at the right time,” said Damian Doherty, editor of a new publication devoted to the field — the Journal of Precision Medicine. His peer-reviewed journal joins an expanding field of similarly focused titles.
It sponsored the Precision Medicine Leaders Summit this month, drawing experts from around the country to downtown San Diego for spirited discussions about the field’s biggest hopes and biggest hurdles.
Tremendous changes have already taken place.
With the use of “big data” and other powerful information technologies, more genetic variations linked to cancer are being identified. Patients’ genomes are screened against drugs such as the blood thinner Plavix to determine if those medications will be effective, a practice pioneered by the local Scripps Health network.
Such testing is also occurring at Rady Children’s Institute for Genomic Medicine in San Diego. Infants and children with undiagnosed diseases are screened there in a bid to find treatments for them. Dr. Stephen Kingsmore, president and CEO of the institute, discussed at the summit how the life of an infant who had seven days to live was saved by this kind of diagnosis.
The summit’s participants also dealt with practical challenges.
These include how to get more Americans from diverse racial, gender and age categories to enroll in clinical trials. Also, how to maximize collaboration between scientific institutes, biotech companies and pharmaceutical giants so there’s a streamlined process for turning lab findings into usable drugs and products.
And the summit’s attendees took on the difficult issue of disparities in access to the most advanced and comprehensive care. In other words, how can experts help patients in poor communities or those living far away from a major medical center secure the chance to try groundbreaking or experimental treatments?
Underlying all of these speeches and forum panels was the omnipresent theme of economics. Can the government, hospitals, physicians, drug companies, scientists and others take advantage of precision medicine to control medical costs while raising the quality of care?
The advantages are too great not to pursue precision medicine, said Euan Ashley, a Stanford University Medical Center associate professor of medicine and genetics, in an article last week in Nature Reviews Genetics.
“Fueled by technological advancement, fundamental discovery of genetic elements related to health and disease has been the engine of human genetics for decades,” Ashley wrote. “Building on this foundation, precision medicine will use the knowledge gained to redefine disease, to realize new therapies and to provide hope for generations of patients to come.”
That’s the vision. At the summit, experts in precision medicine outlined a path to getting there.
Government Efforts
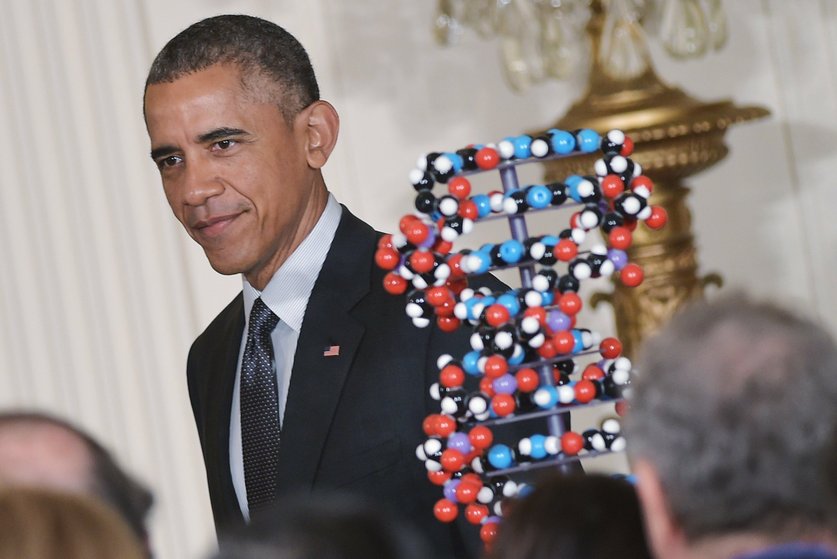
The federal government during President Barack Obama’s tenure and California during Gov. Jerry Brown’s latest terms have committed to advancing precision medicine. These efforts have largely involved fostering coordination among the wide-ranging groups with a stake in the field.
Money hasn’t necessarily been a big part of the governmental investment. California’s initial contribution to precision medicine, announced in 2014, was just $3 million. And the Obama administration’s push came with a relatively modest injection of $215 million.
More important, making precision medicine an official priority gave it a stamp of approval, indicating that this was the direction health care would take. The goal is to get those in all aspects of medicine to understand that they have a role to play, said Dr. Elizabeth Baca, a senior health care adviser in Brown’s Office of Planning and Research.
“It’s not just in one program or one area,” Baca said at the recent summit in San Diego. “It’s about a different approach to disease … the knowledge network, environment, lifestyle. It’s not just about the genes.”
While the $3 million wasn’t a formidable sum, Baca said it served to prompt discussions about how those involved in medicine could use the resources they already have more effectively through translational science.
“We talked with a lot of thought leaders in this space from private sector venture capital, academia, patient groups, to think about what we could do in California,” Baca said.
Since all of this planning is supposed to wind up helping patients, any project adopted by the initiative will be measured for results, Baca said. A benefit to patients needs to show up within two years.
One project selected for funding is to speed up diagnosis of infectious diseases by examining body fluids from the spine and elsewhere for the presence of infectious agents. The fluids are screened for the presence of genetic material from a panel of known pathogens. This technology has already been used to diagnose a disease that numerous tests couldn’t find, Baca said.
The California program’s website is www.ciapm.org.
At the federal level, Obama’s campaign, called the Precision Medicine Initiative, was unveiled in January 2015.
Components include enlisting at least 1 million volunteers to provide their health and genetic information, finding genetic variants that fuel cancer and develop better therapies against them, building high-quality databases and formulating better technology for transmitting data across different networks.
Recruiting the 1 million-plus volunteers started last month.
Safeguarding the privacy of volunteers’ personal information from hackers and others is obviously a concern, said Fae Jencks, a White House adviser with the initiative. The White House is asking the public for suggestions on what it would like to see in terms of data security for such medical projects.
The initiative’s website is whitehouse.gov/pmi.
Since there’s less than half a year left in the White House for the Obama administration, officials have worked to ensure the initiative continues long term, Jencks said. Survival odds look good because Congress has given bipartisan support to the initiative.
The initiative’s work at the National Institutes of Health, the nation’s dominant source of funding for life sciences, is directed by scientist Eric Dishman. The former Intel executive joined the NIH in April. Since he is not a political appointee, Dishman’s job continues even after Obama leaves office, Jencks said.
Cancer
While precision medicine can be used for all diseases, cancer is among those in the most need of better approaches. Uneven progress against cancer provides one of the greatest frustrations for researchers, and it was a major topic at the Precision Medicine Summit.
Underlying the frustration is cancer’s great complexity. It’s not just one disease, but more like many diseases with many different causes. Uncontrolled cell growth is the common factor.
Some forms are easily treatable, such as choriocarcinoma, or cancer of the placenta. This cancer was nearly 100 percent fatal before the discovery of chemotherapy. With chemotherapy, it’s more than 90 percent curable.
Other forms are mostly incurable even today. These include pancreatic cancer, which killed Apple co-founder Steve Jobs at the age of 56. Its five-year survival rate is just 7 percent, according to the American Cancer Society.
Still other cancers, such as ovarian cancer, often initially respond to treatment but tend to recur and metastasize. Subsequent treatments become progressively less effective, and patients often die of the recurrence. Not surprisingly, there’s an urgent push to find more effective drugs for resistant and metastatic cancers, and to get experimental drugs to patients in greatest need.
Many of these newer drugs target genetic disorders specific to tumor cells in particular patients. And existing drugs are being further examined to find out if they may work against other cancers than the ones they are approved to treat.
It’s a promising approach, UC San Diego oncologist and researcher Razelle Kurzrock said at the summit. Kurzrock is co-founder of CureMatch, a San Diego company that makes software that guides doctors in choosing the best course of cancer treatment.
“I genuinely believe that genomics and other ‘omics’ is bringing us the ability to match patients with the best drugs,” Kurzrock said. “What they are telling us is the classical way of doing clinical trials and practice doesn’t work well. And we need to do things differently in order to transform care.”
That transformation must overcome considerable inertia, Kurzrock said.
“We’ve built this enormous way of doing things that we’ve been doing for decades, and the science is saying we need to do things differently,” she said. “For cancer patients with metastatic disease, we need to move to combination therapy. Single agents are unlikely to get very far with these patients.”
Advanced approaches to cancer therapy need to be used earlier in the disease.
“Right now, we’re using them almost exclusively for end-stage patients,” Kurzrock said. “That’s really too late.”
The Clearity Foundation, a San Diego nonprofit, specializes in matching the best drugs to ovarian cancer patients with recurrent tumors. Through partners, Clearity arranges for tumor samples to be genetically analyzed and compared with those of others in a tumor database of hundreds of tumor samples.
Results are summarized in a “tumor blueprint” that indicates which drugs have had the best effect against that tumor’s genetic profile. This can help doctors and patients decide which drugs to try, whether recommended for the cancer, or an “off label” use, or perhaps an experimental drug.
Clearity provides these services free of charge.
Adding To Arsenal
Meanwhile, discoveries continue to roll out, illuminating the molecular roots of cancers.
In June, scientists led by Kurzrock’s fellow researcher and oncologist Catriona Jamieson published a study in the journal Cell Stem Cell that showed how precursor cells to leukemia transform into actual leukemia stem cells — and how that process can be stopped.
The culprit is an enzyme called ADAR1 that edits RNA. In certain leukemias, precursor cancer stem cells become sensitive to inflammation, which causes increased production of ADAR1. That enzyme changes the sequence of genetic molecules called microRNAs.
In turn, the altered microRNAs cause the precursor cells to grow more rapidly, precipitating a dangerous turn of events known as “blast crisis.”
Jamieson said the discovery could be used in the near-term to monitor and predict the progression of leukemia. In the longer term, a drug that can stop the process could be developed to treat ADAR1-sensitive leukemia.
The final link in this process of research for new drugs and development of new ways to use them is to actually get the drugs to patients.
Surgical oncologist Timothy Yeatman told summit participants the clinical trial locations for testing new cancer therapies are inconvenient for many patients who could benefit. These trials tend to cluster in prestigious hospitals in big cities, posing a burden on patients who live far away or who are being treated in community hospitals.
Since 85 percent of cancer care is delivered in these community settings, there’s enormous room to improve patient access, said Yeatman, director of Gibbs Cancer Center. The center is located in Greer, a city of about 27,000 between Greenville and Spartanburg in South Carolina.
Automating start-ups and centralizing contracting can help these community hospitals take part by cutting the needed labor and time, he said.
“You can open a trial up in 17 days from receipt (of authorization) like we did last week,” Yeatman said.
By teaming with community hospitals and their patients, clinical trial sponsors such as drug companies also benefit, Yeatman said, citing a Forbes article on money lost from trials with botched openings.
“Billions of dollars (are) lost in opening trials at sites where there are no patients,” Yeatman said. “If you can screen for patients ahead of time … and then not doing the site visit until you absolutely positively know there’s a patient there … you won’t have goose eggs when you open a trial. And these $100,000 site openings will disappear.”
Advancing Technology
Genomic sequencing and testing technology has progressed exponentially since the first human genome draft was completed in 2001. But everyone in the field agrees that much more progress is needed to truly unlock its potential.
Thermo Fisher Scientific is working toward that end in partnerships with the federal government and pharmaceutical companies, said James Godsey, vice president of R&D for Thermo Fisher’s Clinical Next Generation Sequencing Division.
Thermo Fisher is working with the National Cancer Institute to demonstrate the usefulness of genomic testing as a new standard for guiding treatment, Godsey said. The company has a large center in Carlsbad, acquired when it purchased Life Technologies in a deal completed in 2014 for $13.6 billion. The company competes with Illumina in selling instruments for next-generation sequencing, or NGS.
“Now, the focus is shifting to actionable cancer genes, the identification of those in a very efficient manner,” Godsey said.
For Novartis and Pfizer, Thermo Fisher is developing advanced cancer tests to be used as companion diagnostics for new drugs. This is one way to increase effectiveness by selecting patients whose tumors are genetically vulnerable to specific drugs. Better targeting could also lower prices, by avoiding the use of drugs that are likely to be ineffective.
Getting medicines approved by the U.S. Food and Drug Administration should be easier when accompanied by a test, he said.
“Our goal there is to create the first multi-analyte, universal companion diagnostic NGS panel that enables that,” Godsey said. “The effort is substantial on many fronts. We have to develop the product; the software and the instrumentation, and validate that on their initial (genomic) markers.”
Once that is done, Novartis and Pfizer can simply test their new drugs or drugs from other companies on Thermo Fisher’s FDA-approved 52-gene panel, which quickly detects the presence of thousands of genetic variants associated with solid tumors.
“The time to market approval, the cost, the risk, all is driven down dramatically,” Godsey said. “We think this is central to the success of precision medicine.”
To read this entire article, published online by The San Diego Union-Tribune, please click here.