by Jennifer Southall
Women with mitogen-activated protein kinase-mutated low-grade serous ovarian/peritoneal carcinoma experienced significantly longer PFS and OS compared with women without these mutations, according to study results.
The findings, presented during the Society of Gynecologic Oncology 2022 Annual Meeting on Women’s Cancer, indicate the need to develop novel treatments for women with non-mitogen-activated protein kinase (MAPK)-mutated ovarian cancer, according to the researchers.
Rationale and methods

“We have known for several years that mutations in the MAPK signaling pathway — KRAS, NRAS, BRAF — are common and may occur in approximately half of all low-grade serous ovarian cancers,” David M. Gershenson, MD, professor in the department of gynecologic oncology and reproductive medicine at The University of Texas MD Anderson Cancer Center, and a HemOnc Today Editorial Board Member, told Healio.
“Recent phase 3 clinical trials have shown that women whose low-grade serous carcinoma contains a KRAS/NRAS/BRAF mutation may have a higher probability of response to an agent targeting the MAPK pathway,” Gershenson said. “In 2015, we reported that patients whose tumor contained a KRAS or BRAF mutation by Sanger sequencing appeared to have statistically better OS compared with patients whose tumor did not contain one of these mutations. We were interested in validating this finding with the newer technology of next-generation sequencing.”
The single-institution cohort included 215 women (median age, 46.6 years) with pathologically confirmed low-grade serous ovarian/peritoneal carcinoma and available next-generation sequencing and other adequate clinical data between 2009 and 2020.
Researchers performed multivariable Cox-regression analysis and compared clinical subgroups for PFS and OS.
Key findings
Most women had stage III primary ovarian cancer, with one or more mutations identified in 65.1% (n = 140) of women overall.
Among those with mutations, 97 had a single mutation, 29 had two mutations, 10 had three mutations and four had four mutations. The most common MAPK mutations included KRAS (33%), NRAS (11.2%) and BRAF (8.4%).
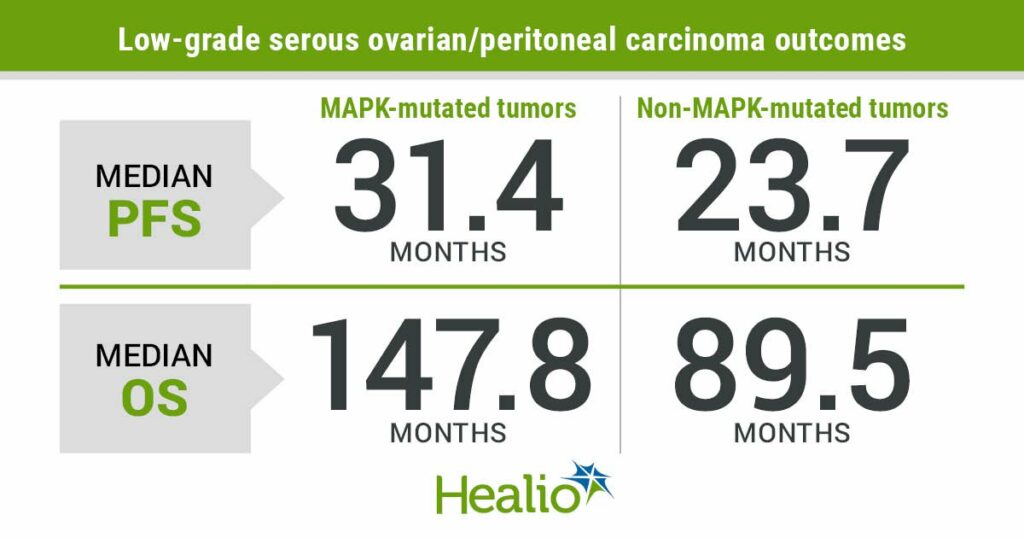
Women with MAPK-mutated tumors (52.6%) experienced significantly longer median PFS (31.4 months; 95% CI, 25.1-37.7) than women without MAPK mutations (23.7 months; 95% CI, 14.1-33.3), as well as significantly longer median OS (147.8 months; 95% CI, 119-176.6 vs. 89.5 months; 95% CI, 61.4-117.7). Those with MAPK mutations also had longer median OS (147.8 months; 95% CI, 119-176.6) than the 75 women without any mutations (78 months; 95% CI, 57.6-98.3). Among 27 women with non-MAPK mutations, researchers reported median OS of 125.1 months (95% CI, 83.9-166.3).
Multivariable analysis showed associations of having a MAPK mutation with longer OS.
A higher proportion of women aged older than 35 years at diagnosis (n = 169) had a MAPK-mutated tumor compared with those aged younger than 35 years (n = 46; 58% vs. 32.6%; P = .002). Women in the younger subgroup had median OS of 86.5 months (95% CI, 71.3-101.8) vs. 136.7 months (95% CI, 114.6-158.8) vs. among the older subgroup (P = .012).
Implications
These findings provide important prognostic information for women with low-grade serous carcinoma of the ovary/peritoneum and their families, Gershenson said.
“Of course, it is also important to emphasize that these observations apply to a large cohort of patients, and there are exceptions to the rule,” he added. “The findings indicate that we need to better understand what drives the pathogenesis of low-grade serous carcinoma beyond mutations in the MAPK signaling pathway. Further research needs to focus on preclinical studies to determine the molecular mechanisms that lead to the development of low-grade serous carcinoma that is not associated with a MAPK pathway mutation. Once we understand this mechanism, we need to develop novel agents to more effectively treat patients without MAPK-mutated tumors.”
This article was published by Healio.