By Amirah Al Idrus
PARP inhibitors have transformed treatment for breast and ovarian cancers, but their use has been limited to the small proportion of patients who have BRCA mutations. New research out of UT Southwestern Medical Center has uncovered a mechanism by which the drugs attack cancer, suggesting they could be put to use in many more patients.
The FDA has approved four PARP inhibitors, starting with AstraZeneca’s Lynparza in 2014 for heavily treated ovarian cancer. These drugs block PARP enzymes, shutting down DNA repair and killing cancer cells. They work in tandem with BRCA mutations, which also hamper DNA repair in cancer cells, delivering a one-two punch that cancer cells cannot survive.
The common wisdom was that cancers needed a BRCA mutation for PARP inhibitors to work.
“PARP inhibitors, like most drugs, started out with a very specific purpose in mind and a very specific molecular mechanism,” said study author W. Lee Kraus, Ph.D., director of the Green Center for Reproductive Biology Sciences at UT Southwestern, in an interview with FierceBiotechResearch. “Their activity was thought to be related to mutations in the genes BRCA-1 and BRCA-2. This became the molecular mechanism that’s all in the realm of DNA damage and DNA repair. The drugs that came [after] Lynparza followed that same process.”
But studies over the years have shown PARP inhibitors work in some patients without BRCA mutations. Kraus’ study provides an explanation for those responses, UT Southwestern said in a statement.
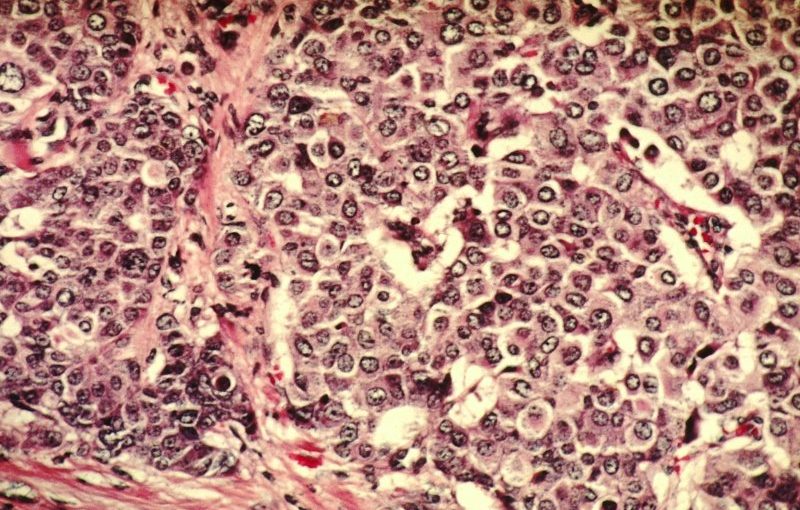
His team found that, in addition to disrupting DNA repair, PARP inhibitors also attack ribosomes, an organelle that makes proteins cancer cells depend on for their explosive growth.
Looking at a wide range of breast cancer cells, Kraus’ team discovered that blocking the PARP-1 protein inhibits a different protein called DDX21, which is found in the cells’ “nucleoli,” special compartments in the nucleus of a cell. Without PARP1, the nucleoli leak DDX21 out into the nucleus, blocking the transcription of ribosomal RNA.
“If you don’t have RNA, you can’t assemble intact ribosomes, and without ribosomes, a lower level of protein translation goes on in the cell. It’s making less protein. And cancer cells are addicted to protein production,” Kraus said. “They are trying to do all of these processes as much as they can, to replicate their DNA, make proteins—all of these things that go into the accelerated growth of the cells. We are just knocking out a different leg from underneath a cancer cell to slow its growth.”
The findings appear in the journal Molecular Cell.
Kraus and his team aren’t alone in their quest to expand the use of PARP inhibitors. Researchers at Yale University are investigating PARP inhibitors and a link between DNA repair and metabolism in two rare, inherited cancers. And scientists at the University of Pennsylvania are looking beyond BRCA mutations by pairing PARP inhibitors with a helper compound: BET inhibitors.
Kraus said that DDX21 could also help identify which patients might respond to PARP inhibitors. “We think that the location of DDX21 in the nucleoli could be an important indicator of whether cells would be responsive to PARP inhibitors,” Kraus said. “But if the protein is already distributed throughout the nucleus, having left the nucleoli, it may not be worth it to treat with PARP inhibitors.”
One limitation of the study is that the team hasn’t yet tested DDX21 as a biomarker. That comes next. Kraus is designing clinical trials with oncologists at UT Southwestern who treat breast and ovarian cancers.
“What we want to do is take patients and maybe group them beforehand—does their cancer had DDX in the nucleoli, or is it more distributed [in the nucleus]? We would look at the efficacy of treatment for those two populations,” Kraus said. “If it works the way we expect it to, it could be a predictor of whether a patient will respond to PARP inhibitors through this particular pathway.”