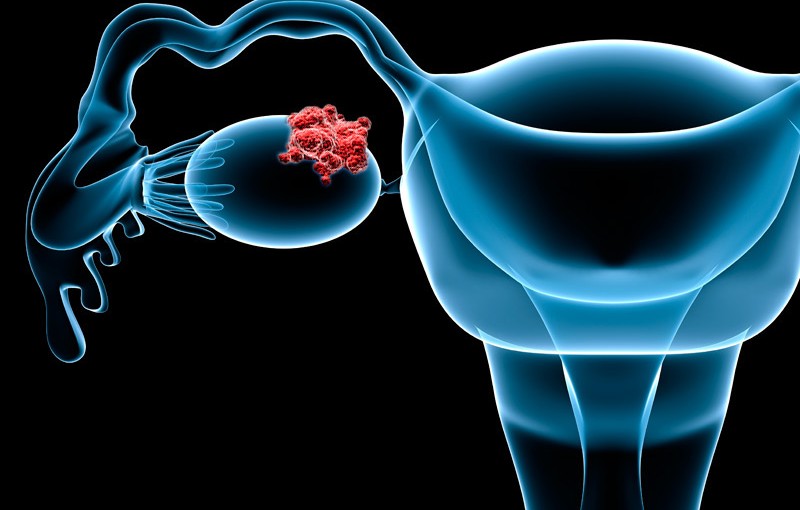
The ovarian cancer treatment paradigm underwent another transformation near the end of 2016 with the FDA approval of the PARP inhibitor rucaparib (Rubraca) for patients with BRCA-positive advanced ovarian cancer who have received at least 2 prior lines of chemotherapy.
The field shifted again when niraparib (Zejula), another PARP inhibitor, was approved in March 2016 as a maintenance treatment for patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy.
The two agents joined the PARP inhibitor olaparib (Lynparza), which was approved in December 2014 for the treatment of women with BRCA-positive advanced disease following treatment with 3 or more prior lines of chemotherapy.
“These drugs allow us to harness [homologous repair deficiency] and give us a chance to kind of use the tumor against itself,” said Lyndsay J. Willmott, MD. “It is kind of a brilliant concept. It makes patients excited that they can actually say ‘I can use this to my advantage’ and, overall, the tolerability is good.”
Next steps, researchers say, involve moving these novel agents into earlier lines of treatment to maximize patient outcomes.
Willmott, a gynecologic oncologist with Arizona Oncology, highlighted the FDA-approved PARP inhibitors and how these approvals have impacted clinical practice and patient outcomes and quality of life in an interview during the 2017 OncLive® State of the Science Summit on Ovarian Cancer.
OncLive: Please provide an overview of your discussion on PARP inhibitors.
Willmott: When you’re talking about PARP inhibitors, the most important thing I think about is the mechanism of action of the drug. The idea about PARP inhibitors is that they’re kind of taking advantage of errors that can happen in patients with ovarian cancer. Essentially, it is using the tumor biology to your advantage. These include some of these repair proteins that allow us to fix DNA damage and they are actually the most perfect repair proteins. Therefore, when we lose these perfect repair proteins, we have to rely on other proteins to make up the difference.
BRCA1/2 and a whole group of other proteins are responsible for what we call homologous repair. We could have mutations in those proteins that can occur in our germline—which are the cells that make up our whole body—or on the tumor itself, which we call somatic. Then, we have to rely on other types of DNA repair. That can include things like nonhomologous end joining. There are a slew of proteins responsible for that, but one of the most important ones are PARP.
The idea is that if we can inhibit these other forms of DNA repair and take the PARP enzyme and make it no longer effective, then this can lead to accumulation of double-stranded breaks. These homologous repair proteins, such as BRCA, normally would fix these. If we don’t have BRCA available, then the cells can’t repair those double-stranded breaks and then they die. That’s the idea behind PARP inhibition.
There have been a number of trials designed to look at PARP inhibitors, and they have been looked at in both the general population—patients who have been previously exposed to chemotherapies—as well as in more modern trials, with the ideas of looking at these treatments as upfront treatment and maintenance. We have also kind of tried to break down to see if patients with BRCA mutations are more likely to benefit from the drug versus the general population.
The first PARP inhibitor that was on the market was olaparib. There have been multiple trials involving this drug, but essentially the current FDA approval is for patients who have received greater than or equal to 3 prior regimens in the setting of a BRCA mutation. This drug has its own companion diagnostic, which is looking at germline mutations.
The second drug, called rucaparib, also recently received FDA approval just in December 2016. That was a slightly different indication, as it’s for patients who received at least 2 prior regimens, again for BRCAmutations. However, this approval also includes patients with somatic mutations. The companion diagnostic for rucaparib actually looks at the tumor and evaluates it for BRCA mutations. If patients have such mutations, then they’re eligible.
The idea behind testing the tumors is that it detects patients with both somatic and germline mutations, so you can capture the entire population. It is important though, for patients who test positive in the tumor, that you go back and test the germline. This is because you can’t really counsel them on things such as other cancer risk—breast cancer risk, for example—or risk to family members. This is because if the mutation exists solely in the tumor, then it doesn’t make them at higher risk for breast cancer, or it doesn’t make their daughter at higher risk for ovarian cancer.
The last drug is called niraparib, and its FDA approval is for maintenance therapy in patients who have platinum-sensitive, recurrent disease who have had a complete response or partial response to their platinum therapy. Then, they can go onto maintenance treatment. The interesting thing about niraparib is that it does not have a companion diagnostic; it’s actually been approved for all patients, regardless of BRCA mutation status.
Do you expect these agents to move up to the frontline setting?
They absolutely can move up to the frontline setting. There are trials actively investigating that, so we’re just waiting on the outcome data to come out. There are even clinical trials right now looking at the combination of PARP inhibitors to cytotoxic therapy—not in the maintenance setting but literally right after surgery or in neoadjuvant fashion.
Prior trials that have evaluated PARP inhibitors given that way have had a lot of toxicity issues. However, it is still an interesting question. Can we give a PARP inhibitor in an effective and safe way to the cytotoxic chemotherapy and does it improve outcomes?
Can we combine PARP inhibitors with immunotherapy agents?
Yes. The immunotherapy world is evolving right now, so there are a lot of future combinations. I am certain that immunotherapy will be given, so we need to establish that immunotherapies are effective in ovarian cancer.
There are big trials. The JAVELIN Ovarian 200 trial is specifically looking at avelumab (Bavencio) in addition to cytotoxic chemotherapy. Once we establish that they are effective in a large phase III trial, then we will start to look at combinations.
The recent approvals of rucaparib and niraparib have led to a lot of excitement in the field. Anecdotally, how have you seen these agents impact clinical practice?
Patients are happy with the idea that they can take an oral drug. The biggest toxicities that we monitor for are hematologic, in addition to gastrointestinal (GI). For GI toxicities, if you can send your patient home with a prescription for an antinausea or antidiarrheal medicine and they can take that medicine at the first sign of a symptom, then that gives them some control over those side effects and make them acceptable.
Hematologic toxicities can be a little bit more complicated, and there are a number of ways of dealing with these toxicities. For example, we can treat through the anemia and give a transfusion as necessary versus short-term dose delays. The fatigue can be a greater issue but, for some patients, that can be improved by dose modifications.
Overall, patients do appreciate the flexibility of not having to come in for their infusion and feeling like they have a little more autonomy and not so much dependence upon coming into the office.
To read this entire article in The Clearity Portal, please click here.