NEW YORK – Data from a Phase I study published last week in the Journal of Clinical Oncology showed that Bayer’s investigational compound anetumab ravtansine (BAY 94-9343), an antibody-drug conjugate comprising an anti-mesothelin antibody linked to maytansinoid DM4, was well tolerated in patients with advanced, metastatic, or recurrent solid tumors that expressed the tumor-differentiation antigen mesothelin.
The data also indicated “a positive trend,” suggesting that high mesothelin expression may be useful for predicting which cancer patients will benefit from anetumab ravtansine.
The study, led by Raffit Hassan of the National Cancer Institute, enrolled 148 patients with solid tumors. Tumor response was evaluated in 138 of the 148 patients enrolled in the study. Overall, 66 patients had stable disease, 11 patients had a partial response, and one patient achieved a complete response.
The overall response rate was 16 percent in the 6.5 mg/kg once-every-3-weeks dosing cohort, 9 percent in the 1.8 mg/kg once-per-week dosing cohort, and 6 percent in the 2.2 mg/kg once-per-week dosing cohort. The disease control rate was 65 percent, 54 percent, and 64 percent, respectively. In the ovarian cancer subgroup, one patient achieved complete response at the 2.2 mg/kg once-per-week dosage.
The highest overall response rate of 31 percent was observed in the 6.5 mg/kg once-every-3-weeks mesothelioma subgroup. Disease control rate in this group was 75 percent.
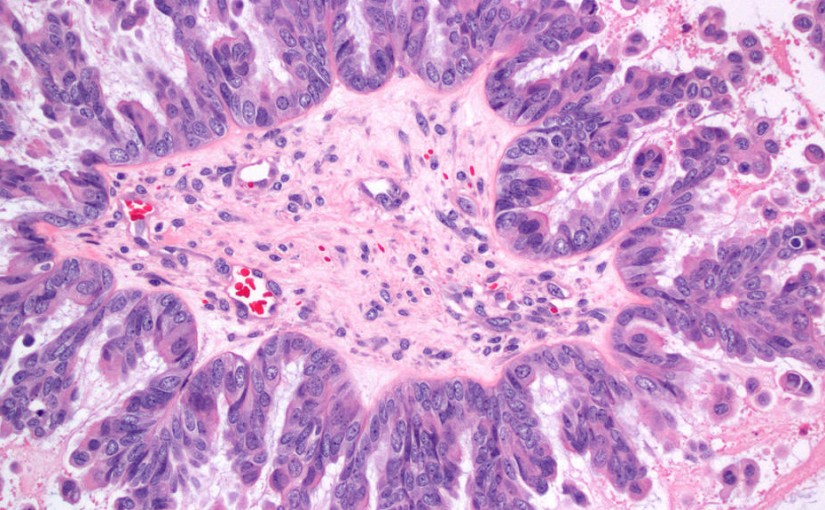
All patients with an observed partial response and complete response had at least 60 percent tumor mesothelin expression as detected by an immunohistochemistry test.
Using results observed from the trial, investigators set the maximum tolerated dose of anetumab ravtansine at 6.5 mg/kg once every three weeks or 2.2 mg/kg once per week. There were no drug-related deaths observed in the study.
Anetumab ravtansine binds to the mesothelin on tumor cells and is internalized, which releases DM4. DM4 binds to tubulin, which can arrest cell cycle and trigger cell death. The release of DM4 into the tumor microenvironment can also kill any neighboring dividing cells.
Hassan and colleagues noted that “while all patients who responded to treatment had high mesothelin expression, some patients with high mesothelin expression did not respond to treatment. These findings suggest that, although there is a positive trend in the correlation between mesothelin expression and antitumor activity, significance cannot be established on the basis of the preliminary data from this study.”
Mesothelin is a transmembrane tumor differentiation antigen that is highly expressed in many solid tumors. It is found in around 85 percent to 95 percent of mesotheliomas, 80 percent to 85 percent of pancreatic cancers, 60 percent to 65 percent of ovarian cancers, 57 percent to 64 percent of non-small cell lung cancers, 50 percent to 55 percent of stomach cancers, and 25 percent to 30 percent of breast cancers. It is hypothesized to be important for tumor implantation and metastasis. Previous research has found that mesothelin expression in normal tissues is limited.
Several additional trials of anetumab ravtansine are underway evaluating the drug as monotherapy or in combination with standard of care in a variety of mesothelin-expressing solid tumors. This includes anetumab ravtansine in combination with pegylated liposomal doxorubicin in recurrent mesothelin-expressing platinum-resistant cancer, anetumab ravtansine and atezolizumab (Genentech’s Tecentriq) in mesothelin-expressing non-small cell lung cancer, anetumab ravtansine with and without pembrolizumab (Merck’s Keytruda) in mesothelin-positive pleural mesothelioma, and a basket trial of anetumab ravtansine in mesothelin-expressing advanced solid tumors.
This article was published by Precision Oncology News.